Mr. Zhang, a 55-year-old construction worker, suffered from hepatitis B for more than 30 years. His condition began to worsen three years ago, as he began to feel more and more tired and to show edema (e.g face, leg). Unfortunately, the disease had progressed to the stage of liver cirrhosis.
As Mr. Zhang’s condition became more and more serious, complications included gastric fundus esophageal varices, edema of lower limbs and ascites, which seriously affected his everyday life.
A liver transplant was his only hope. However, liver donors are very scarce. In China, most of the liver sources are from patients with brain death caused by accident. Relative to the vast number of patients waiting for liver transplantation in China, donors are not enough.
Mr. Zhang was lucky enough to have a donor with the same blood type. He and his family were thrilled because it meant being born again, but he had no idea of the difficulties ahead.
Liver transplantation is a complicated surgery with high risk. Completing surgery is only the first step in the treatment process, and postoperative complications include infection, rejection, bleeding, vascular stenosis and thrombosis. The occurrence of any complications can directly cause failure of transplantation.
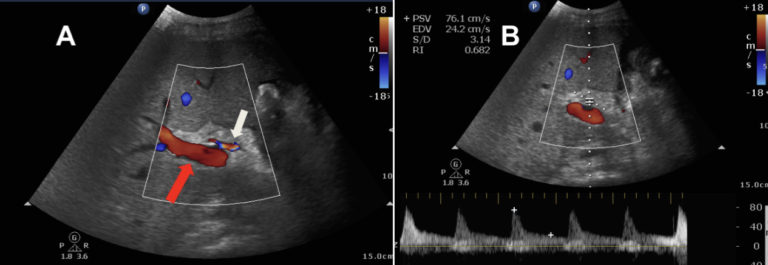
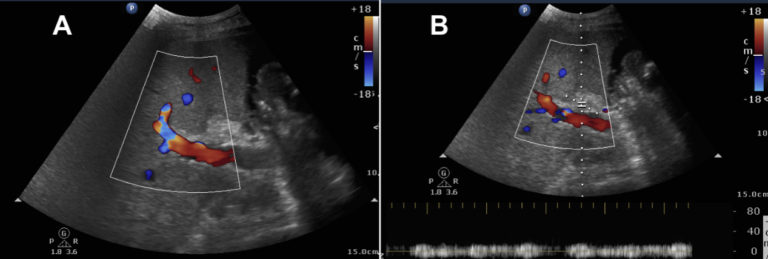
On fourth day after Mr. Zhang’s liver transplantation, surgeons received bad news that the blood flow and spectrum of the hepatic artery were difficult to detect,and there was a significant increase in glutamic-pyruvic transaminase and glutamic-oxalacetic transaminase. Surgeons determined that postoperative hepatic artery stenosis and occlusion led to ischemic injury of the liver.
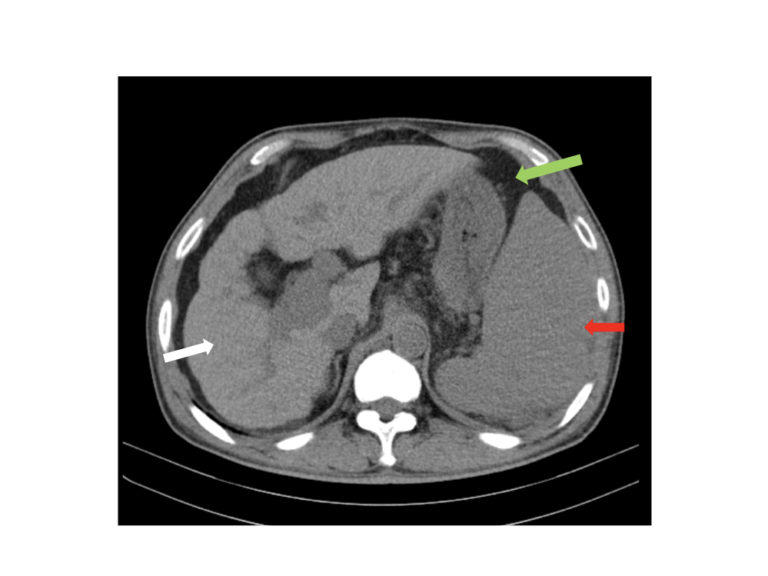
The surgeons initially decided to perform enhanced CT for Mr. Zhang. However, as his condition worsened, his blood creatinine was too high for an enhanced CT scan. After consultation with radiologists, the team decided to administer a contrast-enhanced ultrasound (CEUS) scan of the liver. CEUS does not have hepatorenal toxicity and could provide real-time blood flow perfusion of liver vessels.
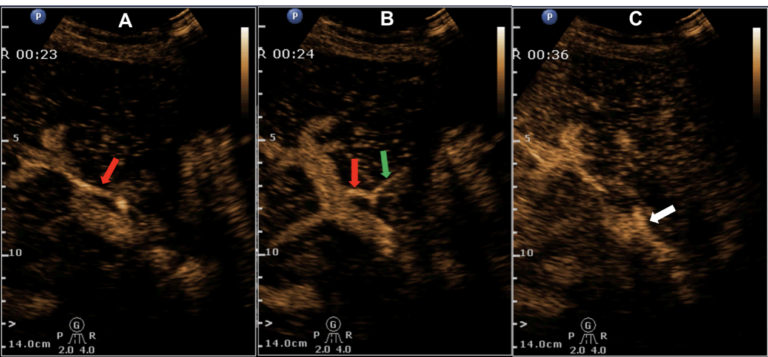
Fortunately, CEUS clearly showed the hepatic artery perfusion; the ultrasoaund contrast was well observed in both the right and left hepatic arteries. This showed that the original diagnosis of postoperative hepatic artery stenosis and occlusion was incorrect.
Mr. Zhang learned the good news at the end of his CEUS exam. Later, surgeons found that hypoproteinemia was causing the liver’s Gleason sheath edema, which reduced blood supply to the hepatic artery. A conventional ultrasound examination would not have been able to detect the blood flow or confirm the correct diagnosis. Ultimately, after hepatic functional protection, Mr. Zhang’s liver function gradually recovered.
Thanks to a relatively quick and easy CEUS exam, Mr. Zhang received a reliable diagnosis, which avoided the risk of renal impairment associated with enhanced CT, and with the correct diagnosis prevented the possibility of a second operation.
As Mr. Zhang’s experience shows, the application of CEUS can effectively help clinicians make an accurate judgment and treatment plan which significantly benefits patients.

