David is a 32-year old man with Down syndrome and a congenital ventricular septal defect, a cardiac abnormality. Despite technically successful cardiac surgery in childhood, David developed heart failure, chronic liver congestion and a chronic blockage of the portal vein, the main vessel draining the intestinal blood into the liver. Repeated fluid taps showed chylous ascites, a form of fluid buildup suggesting a lymphatic leak.
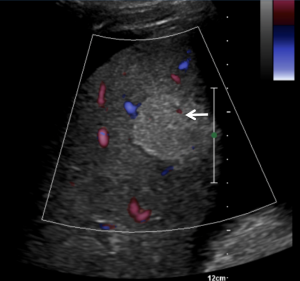
Ultrasound of the abdomen was performed to look for causes of the fluid leak. The images showed large ascites and mild nodularity of the liver contour, raising suspicion of cirrhosis, in this context likely of cardiac origin. In addition, a homogenously echogenic round area of hepatic parenchyma was noted in the right lobe, raising suspicion of a mass suggestive of liver cancer given cirrhotic appearance of the liver. (Fig. 1).

Color Doppler demonstrated little flow in that area, which was non-specific and therefore did not add to finding the diagnosis. (Fig. 2)
Contrast-enhanced MR and CT were then used to further evaluate the area of suspicions, but images were of limited quality in both cases due to David’s inability to hold his breath.
Finally, contrast enhanced ultrasound (CEUS) was used to further characterize the mass, and David’s mother was in the room as the scan was performed.
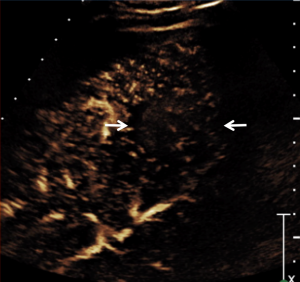
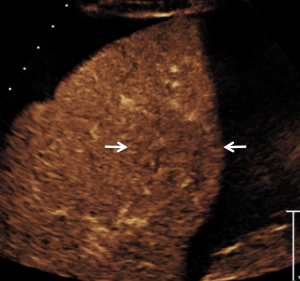
CEUS produced excellent images without requiring David to hold his breath and in addition, the diagnosis was immediate. CEUS demonstrated slightly decreased vascularity of the lesion on all contrast phases (arterial phase: Fig. 3; venous phase: Fig. 4) compared to surrounding parenchyma. Further, there was no distortion of normal vessels; this contrast enhancement pattern was typical for a benign portion of liver regeneration containing some fat associated with cardiac cirrhosis, a so-called regenerating nodule.
A biopsy was performed for further reassurance, and the histologic assessment confirmed normal liver with fatty infiltration and no tumor, typical for benign regenerating nodule. In addition, no cirrhosis was found.
Although the etiology of the lymphatic leakage was not determined, the most likely cause of the chylous ascites was portal hypertension as a complication of portal vein occlusion.
David and his mother appreciated the immediate diagnosis with CEUS, confirmed by benign biopsy results received a few days later.
Now, one year later, David continues to be monitored and treated for recurrent ascites and weight loss, both known complications of lymphatic leakage and protein loss associated with congestive liver disease and portal hypertension. However, due to the use of CEUS and the biopsy proven absence of cirrhosis, there is no need to worry about liver cancer…

