Body Imaging – Liver
- Liver Intro
- Liver Contrast
- Exam Protocol
- Image Gallery
- Guidelines
- Bibliography
CEUS is a safe, versatile and reliable tool for imaging the liver in the following clinical contexts:
- Characterization of focal liver lesions
- Resolution of indeterminate masses from CT and MR scans
- Guide interventional procedures
- Follow-up interventional procedures
- Assessment of liver vascularity
- Monitor changes in enhancement pattern over time for selected LR-3 or LR-4 observations
- Differentiate tumor in vein from bland thrombus
CEUS uses ultrasound contrast agents (UCAs) to improve the clarity and reliability of conventional ultrasound scans. UCAs are comprised of liquid suspensions of biodegradable gas-filled microspheres (sometimes called “microbubbles”). When they are injected into a patient’s arm vein during an ultrasound exam, they flow through the body’s microcirculation without impediment, and are metabolized and expelled from the body within minutes.
Details on “how to” below:
Patricia C. Jo, MD Hyun-Jung Jang, MD Peter N. Burns, PhD Kelly W. Burak, MD Tae Kyoung Kim, MD Stephanie R. Wilson, MD
Integration of Contrast enhanced US into a Multimodality Approach to Imaging of Nodules in a Cirrhotic Liver: How I Do It
Radiology: Volume 282: Number 2—February 2017 317 – 331.
Commonly asked CEUS questions
Timing: Imaging and timer begins with the start of the saline flush. Continuous recording from the arrival of the first bubble in the FOV to just beyond the peak of maximum enhancement (approximately 20-60 sec). Stop imaging (leave transducer in place) and then follow with intermittent brief acquisitions (5-10 sec) every 30 or 60 seconds for up to 5-6 minutes. Shorter scanning may be appropriate if the lesion is fully characterized sooner. In the PVP and late phases, a sweep of the liver can be performed to evaluate for additional lesions (looking for wash-out). From the cine clips, still images can then be saved at the end of the study.
Tips: Utilize the shortest distance from the transducer crystal to the lesion to optimize the study. Consider supine and LLD patient positions and also subcostal and intercostal transducer placement. Imaging in the long axis of the patient will generally reduce out of plane images due to respiration. Practice breathing with the patient utilizing either quiet breathing or breath suspension in neutral position over full suspended inspiration.
Hepatocellular Carcinoma
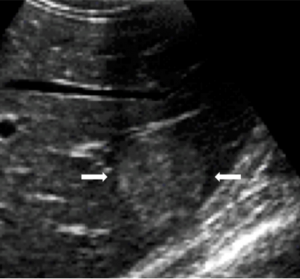
The appearance of hepatocellular carcinoma (HCC) on greyscale and color Doppler ultrasound non-specific.
The typical finding of hepatocellular carcinoma (HCC) on CEUS is a hypervascular mass on arterial phase with gradual loss of enhancement (“washout”). Washout is slower and less pronounced than with cholangiocarcinoma or metastases.
Some HCC however don’t demonstrate hypervascularity or washout.
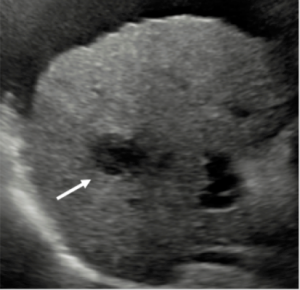
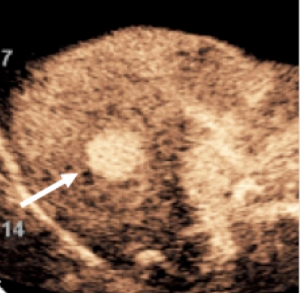
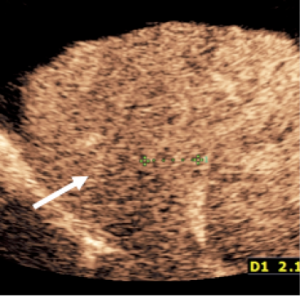
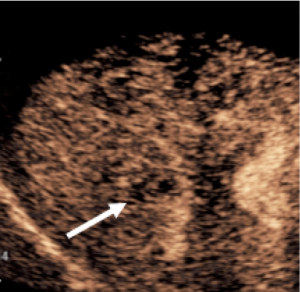
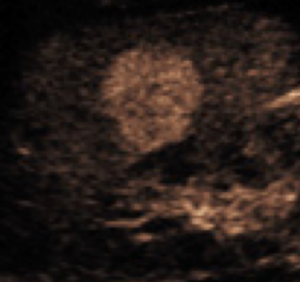
Hepatocellular Carcinoma on surveillance in cirrhosis
CEUS diagnosis of a nodule found on surveillance ultrasound in a patient at risk for development of hepatocellular carcinoma (HCC) due to cirrhosis.
The sequence of events demonstrated below is diagnostic of HCC. No biopsy is required for the diagnosis.
Typical CEUS findings of HCC are early hypervascular enhancement and gradual washout of contrast after one or several minutes.
The patient may be treated while the tumor is still small and amenable to treatment.
Courtesy Dr. Stephanie R Wilson, University of Calgary
Focal Nodular Hyperplasia (FNH)
The appearance of a focal nodular hyperplasia (FNA) on greyscale ultrasound is mostly isoechoic to liver, but often variable. The classic finding on color Doppler ultrasound is the “spoke wheel” artery, which is a central or eccentric artery with centrifugal flow. However this finding is not always seen on color Doppler.
CEUS shows the spoke wheel artery more reliably with rapid radial flow and homogenous enhancement of the lesion within a few seconds and sustained enhancement later.
Focal Nodular Hyperplasia (typical)
Incidental finding of a subtle small well-defined mass in the liver next to the kidney with rapidly enhancing central “spoke wheel artery”, typical for focal nodular hyperplasia (FNH). This finding is diagnostic for FNH and no further work-up or follow-up of this benign finding is necessary.
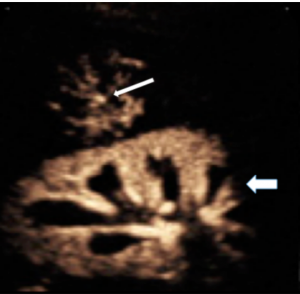
Courtesy Dr. Stephanie R Wilson, University of Calgary
- Liver Imaging Reporting and Data System Contrast-Enhanced US Nonradiation Treatment Response Assessment Version 2024
- Barr, Richard G., et al., Society of Radiologists in Ultrasound (SRU): Contrast-enhanced Ultrasound—State of the Art in North America Ultrasound Quarterly: September 2020 – Volume 36 – Issue 4S – p S1-S39 doi: 10.1097/RUQ.0000000000000515
- Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver – 2ndrevision April 16, 2020; A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS.
- Lyshchik A, Kono Y, Dietrich CF et al. Contrast-enhanced ultrasound of the liver: technical and lexicon recommendations from the ACR CEUS LI-RADS working group. Abdom Radiol (NY). 2018 Apr;43(4):861-879
- CEUS LI-RADS v2017 – American College of Radiology
Barr, R.G., Contrast enhanced ultrasound for focal liver lesions: how accurate is it? Abdom Radiol (2018) 43:1128–1133
Darge, K., et al., Safety of contrast-enhanced ultrasound in children for non-cardiac applications: a review by the Society for Pediatric Radiology (SPR) and the International Contrast Ultrasound Society (ICUS). Pediatr Radiol, 2013. 43(9): p. 1063-73.
Burns, P.N., S.R. Wilson, and D.H. Simpson, Pulse inversion imaging of liver blood flow: improved method for characterizing focal masses with microbubble contrast. Invest Radiol, 2000. 35(1): p. 58-71.
Wilson, S.R. and P.N. Burns, An algorithm for the diagnosis of focal liver masses using microbubble contrast-enhanced pulse-inversion sonography. AJR Am J Roentgenol, 2006. 186(5): p. 1401-12.
Burns, P.N. and S.R. Wilson, Focal liver masses: enhancement patterns on contrast-enhanced images–concordance of US scans with CT scans and MR images. Radiology, 2007. 242(1): p. 162-74.
Durot, I., S.R. Wilson, and J.K. Willmann, Contrast-enhanced ultrasound of malignant liver lesions. Abdom Radiol (NY), 2017.
Jang, H.J., T.K. Kim, and S.R. Wilson, Small nodules (1-2 cm) in liver cirrhosis: characterization with contrast-enhanced ultrasound. Eur J Radiol, 2009. 72(3): p. 418-24.
Jang, H.J., et al., Enhancement patterns of hepatocellular carcinoma at contrast-enhanced US: comparison with histologic differentiation. Radiology, 2007. 244(3): p. 898-906.
Jo, P.C., et al., Integration of Contrast-enhanced US into a Multimodality Approach to Imaging of Nodules in a Cirrhotic Liver: How I Do It. Radiology, 2017. 282(2): p. 317-331.
Claudon, M., et al., Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver – update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med Biol, 2013. 39(2): p. 187-210.
Piscaglia, F., et al., The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med, 2012. 33(1): p. 33-59.
Wilson, S.R., et al., Enhancement patterns of focal liver masses: discordance between contrast-enhanced sonography and contrast-enhanced CT and MRI. AJR Am J Roentgenol, 2007. 189(1): p. W7-W12.