Body Imaging – Kidney
- Kidney Intro
- Exam Protocol
- Image Gallery
- Guidelines
- Bibliography
CEUS is a safe, versatile and reliable tool for imaging the kidney in the following clinical contexts:
- Characterization of indeterminate renal masses
- Evaluation of renal parenchyma in patient with suspected renal abscess
- Evaluation of renal transplants in patients with suspected renal vascular complications and renal infarcts
- Follow-up of non-surgical renal lesions
- Guide interventional procedures
- Follow-up interventional procedures
CEUS uses ultrasound contrast agents (UCAs) to improve the clarity and reliability of conventional ultrasound scans. UCAs are comprised of liquid suspensions of biodegradable gas-filled microspheres (sometimes called “microbubbles”). When they are injected into a patient’s arm vein during an ultrasound exam, they flow through the body’s microcirculation without impediment, and are metabolized and expelled from the body within minutes.
Dr. Richard G. Barr, Commonly asked CEUS questions
Imaging and timer begin with the start of the saline flush. Continuous recording from first arrival of a bubble in the FOV to lesion characterization, which usually less than 2- minutes. From the cine clips, still images can then be saved at the end of the study. Scanning the entire lesion particularly in indeterminate masses is required. Often scanning the kidney for additional lesions is possible.
CONTRAST AGENT DOSING: Depends on transducer and instrumentation, and body habitus. In general, for adult patients, a dose of 1.5-2.4 ml Lumason; Definity 0.2-0.4ml; Optison 1.0-1.5ml
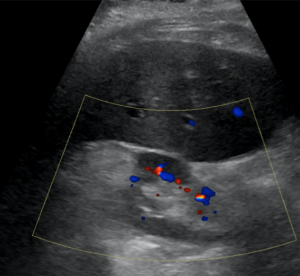
Angiomyolipoma
Echogenic appearance on grey scale ultrasound and absence of color flow despite hypervascularity is typical, but not specific for angiomyolipomas (AML). CEUS can help identifying hypervascularity mixed with hypovascular components, typical for AML. Necrotic non-enhancing components are not typical for AML.
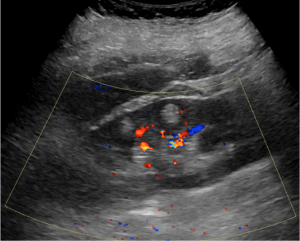
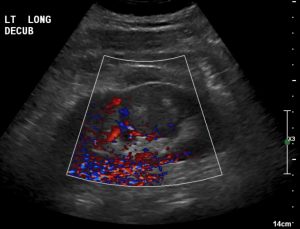
Angiomyolipoma (mixed vascularity)
Partly exophytic echogenic kidney mass is peripherally rapidly enhancing after contrast administration, while demonstrating hypovascular enhancement centrally, which persists on later contrast phases.
Courtesy Dr. Richard Barr, Northeast Ohio Medical University
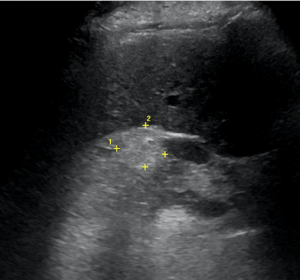
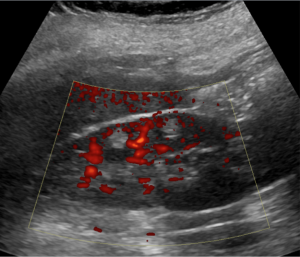
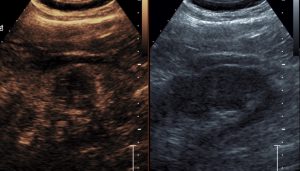
Angiomyolipoma (hypovascular)
81-year old woman with incidental finding of two small echogenic intracortical angiomyolipomas (AML). The tumors are hypovascular and are barely enhancing after contrast administration, which is typical for small AML.
Courtesy Dr. Richard Barr, Northeast Ohio Medical University
Renal Cell Carcinoma
The most common and aggressive type of renal cell carcinoma is the clear cell type. While the histologic subtypes of renal cell carcinomas cannot be distinguished on conventional ultrasound, it can often be characterized by CEUS: clear cell carcinomas are typically hypervascular and may show compartments of necrosis, while papillary and chromophobe carcinomas are usually uniformly hypovascular. With CEUS tumor thrombi within renal veins can also be more confidently detected.
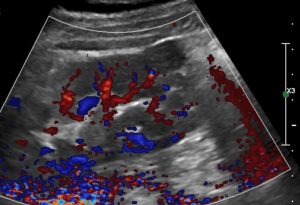
Clear Cell carcinoma
Typical clear cell carcinoma with strong irregular peripheral enhancement after contrast administration comparable to renal cortex. There is central non-enhancing necrosis. Hypervascular portions demonstrate washout (hypoechoic appearance compared to renal parenchyma) on late phase, which is also typical.
Courtesy Dr. Richard Barr, Northeast Ohio Medical University
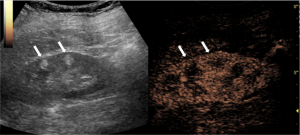
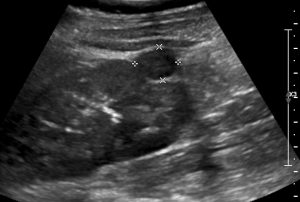
Cystic Renal Cell Carcinoma
Cystic mass with irregular septations, which is a non-specific finding on greyscale ultrasound as this appearance may be seen with benign complex as well as with cystic malignancies.
CEUS demonstrates strong enhancement and reveals additional nodularities within the septations, which excludes a benign complex cyst. Mass was removed and pathology revealed cystic clear cell renal carcinoma.
Courtesy Dr. Richard Barr, Northeast Ohio Medical University
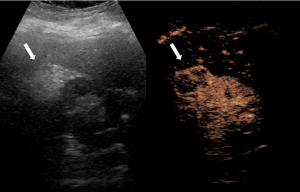
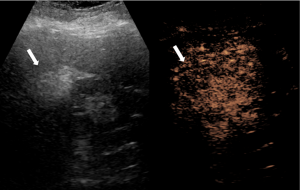
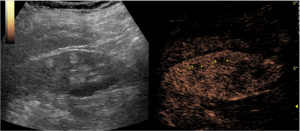
Papillary Renal Cell Carcinoma
Incidental finding of a small exophytic renal tumor, which is hypoechoic on greyscale ultrasound and non-specific. A complex cyst can therefore not be distinguished from a solid tumor.
CEUS demonstrates uniform weak enhancement with washout on the late phase, which is typical for papillary carcinoma, confirmed by excision. A complex cyst as well as a more aggressive clear cell carcinoma could therefore be ruled out.
Courtesy Dr. Richard Barr, Northeast Ohio Medical University
- Barr, Richard G., et al., Society of Radiologists in Ultrasound (SRU): Contrast-enhanced Ultrasound—State of the Art in North America Ultrasound Quarterly: September 2020 – Volume 36 – Issue 4S – p S1-S39 doi: 10.1097/RUQ.0000000000000515
- Piscaglia, F., et al., The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med, 2012. 33(1): p. 33-59.
- Sidhu PS., et.al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017. Ultraschall in Med 2018; 39: e2–e44.
Barr RG. How to Develop a Contrast-Enhanced Ultrasound Program. J Ultrasound Med 2017.
Barr RG, Peterson C, Hindi A. Evaluation of indeterminate renal masses with contrast-enhanced US: a diagnostic performance study. Radiology 2014;271; 133-142.
Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsoe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC, Chaubal NG, Chen MH, Clevert DA, Correas JM, Ding H, Forsberg F, Fowlkes JB, Gibson RN, Goldberg BB, Lassau N, Leen EL, Mattrey RF, Moriyasu F, Solbiati L, Weskott HP, Xu HX. Guidelines and Good Clinical Practice Recommendations for Contrast Enhanced Ultrasound (CEUS) in the Liver – Update 2012. Ultraschall Med 2012.
Dietrich CF, Ignee A, Hocke M, Schreiber-Dietrich D, Greis C. Pitfalls and artefacts using contrast enhanced ultrasound. Z Gastroenterol 2011;49; 350-356.
Fetzer DT, Rafailidis V, Peterson C, Grant EG, Sidhu P, Barr RG. Artifacts in contrast-enhanced ultrasound: a pictorial essay. Abdom Radiol (NY) 2018;43; 977-997.
O’Neal D, Cohen T, Peterson C, Barr RG. Contrast-Enhanced Ultrasound-Guided Radiofrequency Ablation of Renal Tumors. J Kidney Cancer VHL 2018;5; 7-14.
Piscaglia F, Nolsoe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O, Claudon M, Clevert DA, Correas JM, D’Onofrio M, Drudi FM, Eyding J, Giovannini M, Hocke M, Ignee A, Jung EM, Klauser AS, Lassau N, Leen E, Mathis G, Saftoiu A, Seidel G, Sidhu PS, ter Haar G, Timmerman D, Weskott HP. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 2012;33; 33-59.
Tenant SC, Gutteridge CM. The clinical use of contrast-enhanced ultrasound in the kidney. Ultrasound 2016;24; 94-103.
Sparchez, Z., et al., Contrast enhanced ultrasound of renal masses. A reappraisal of EFSUMB recommendations and possible emerging applications. Med Ultrason, 2015. 17(2): p. 219-26.
Sidhu, P.S., et al., The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med, 2018. 39(2): p. e2-e44