Susan* is a 20-year-old patient with a rare genetic form of bone marrow failure known as dyskeratosis congenita (DC). Her condition is caused by a mutation of the TERC gene, which normally provides instructions for making a component of an enzyme that is essential for cell survival. Susan’s DC prevents her marrow from producing sufficient blood cells.
Approximately 25 days after a bone marrow transplant, while Susan was hospitalized and awaiting engraftment, she experienced progressive abdominal bloating (distension), nausea, and back and abdominal pain. These symptoms persisted for several days.
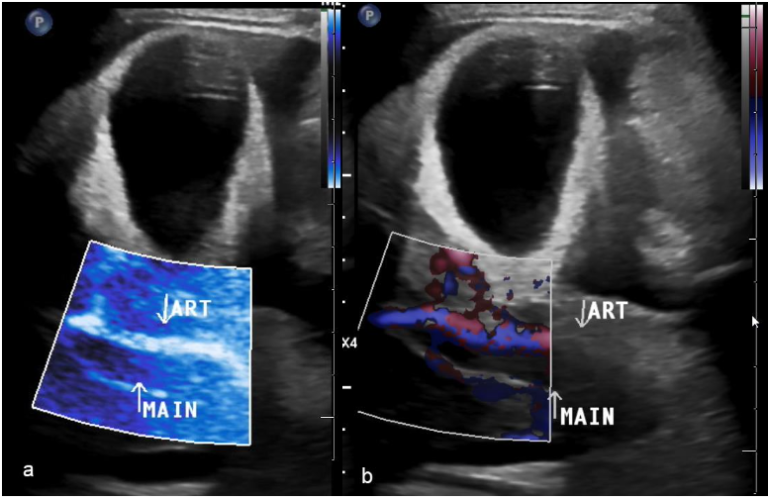
Susan’s doctors initially performed a conventional ultrasound scan to evaluate her for veno-occlusive disease (VOD), a complication that can occur after bone marrow transplant where the small veins in the liver become blocked. The scan showed moderate volume ascites, gallbladder wall thickening and acute thrombosis of the portal vein. Blood flow could not be detected in the main portal vein or its branches on grayscale, color or power Doppler, or MicroFlow imaging. (Figure 1)
Given these findings, the pediatric interventional radiology (IR) team was asked to consider removal of a blood clot in Susan’s portal vein – i.e., a thrombectomy. This procedure involves sticking a needle through the liver and into the portal vein. For Susan, there would be additional risk due to her immunocompromised status and lower-than-normal red and white blood cells and platelets (pancytopenia).
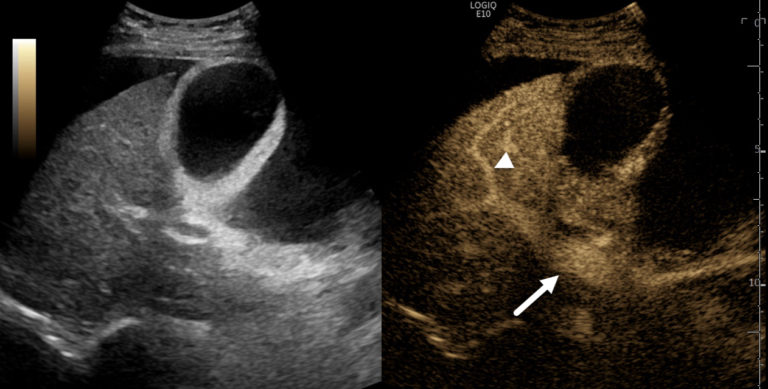
To re-evaluate the portal vein, Susan’s doctors performed a contrast enhanced ultrasound (CEUS) scan in the IR suite. The administration of an ultrasound contrast agent showed normal enhancement of the main portal vein and intrahepatic branches with normal flow in the direction of the liver. (Figure 2) In addition, CEUS showed that there were no filling defects or other findings of portal vein blood clots.
Fortunately for Susan, these CEUS results allowed her to avoid a potentially risky interventional procedure and, instead, be medically managed for presumed VOD. In addition, CEUS helped her doctors identify extremely slow flow in her portal vein. While CT might have been another imaging option for this young patient, CEUS was preferable because Susan was at increased risk of radiation-induced damage due to her underlying diagnosis of DC.